
Posted October 7, 2022
Microglia are the innate immune cells that reside in the central nervous system and remove unwanted particles and debris from the brain. TREM2 is a receptor found on microglia and its activation increases amyloid beta uptake; the effect is therefore neuroprotective. An antibody designed to increase TREM2 activation has shown therapeutic promise in the lab by decreasing the pathology of the disease. A single antibody injection induced microglia proliferation and converted them into an active state. Additional injections reduced plaque formation and the resulting damage to neurons. Phase 1 clinical trials of antibody activation of TREM2 are currently in process.
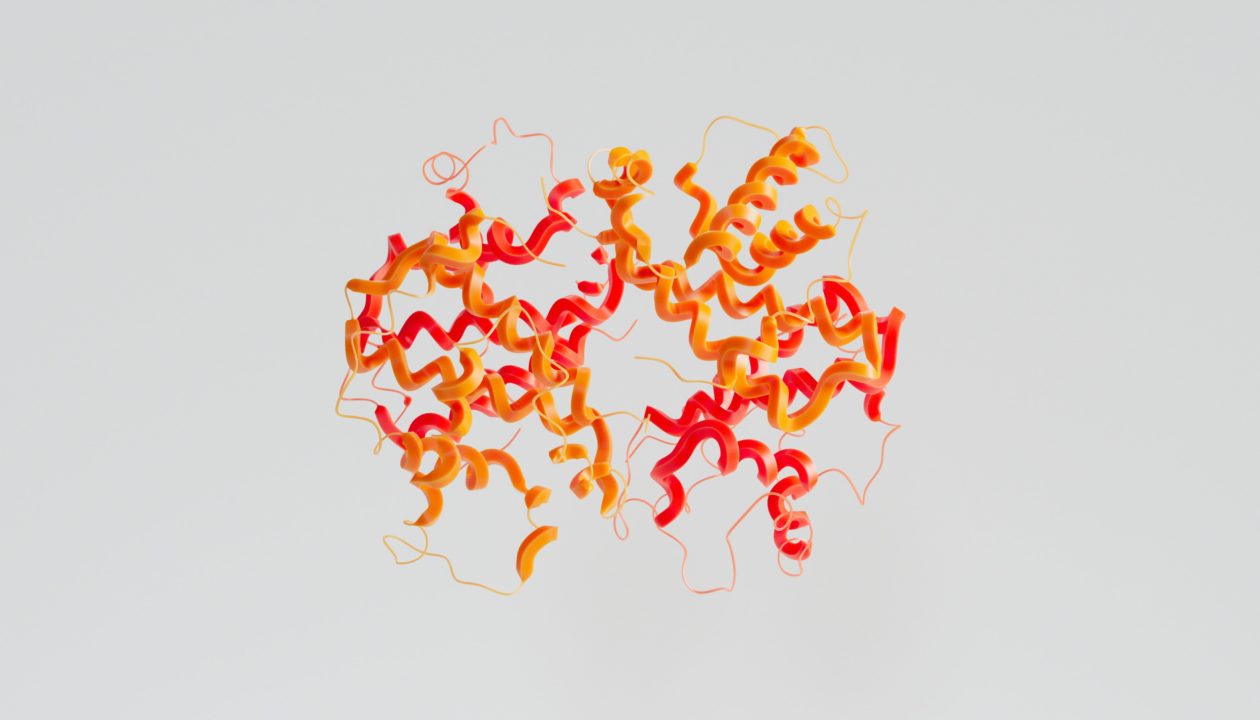
Microglia are the innate immune cells of the brain; they monitor the brain for signs of viruses, bacteria, and cellular debris, including amyloid beta. When pathogens or toxins are detected, microglia become activated and ingest the particles, removing the toxins from the brain.
In a paper published in the Journal of Experimental Medicine, researchers led by Marco Colonna, M.D., a member of the Cure Alzheimer’s Fund’s Research Leadership Group, developed an antibody for the TREM2 receptor on microglia that activated microglia in a mouse model of AD, reducing the number of neurotoxic plaques and damaged or dying neurons. Following the procedure, behavioral changes were noticed and the AD mice behaved more like their counterparts who did not have amyloid beta pathology. A variant of the antibody is being tested in a first-in-human Phase I clinical trial and has proven to be well-tolerated with no serious adverse side effects.
TREM2 is a receptor found on microglia that, when stimulated, cause the microglia to proliferate and become active. Colonna’s group created an antibody (AL002c) that could stimulate TREM2 receptors. Since certain mutations in TREM2 have been found to increase the risk for AD, the lab wanted to investigate if the TREM2 antibody could stimulate microglia in the TREM2 receptor with mutations. Therefore, they tested the antibody in two mouse models of AD, which expressed mutated TREM2. These mice developed amyloid beta plaques at a young age, and all antibody treatments were tested after amyloid beta aggregation and plaque formation.
A single antibody injection resulted in the proliferation and activation of microglial cells, demonstrating that the antibody can stimulate TREM2 activity despite the receptor having mutations.
Next, the researchers tested the effect of prolonged antibody exposure by injecting mice weekly for three months. Subtle but significant changes were noted in the behavior of the mice during an Elevated Plus Maze test. In this test, a plus-shaped maze is elevated three feet off the floor. Two arms of the maze are open with no walls, while the other two are walled. This test assesses risk-taking behavior, exploratory drive, and anxiety-like traits. Typically, mice will spend more time exploring the walled arms of the maze and avoid the open arms. Before antibody treatment, the mice spent more time exploring the open arms of the maze. This suggested that amyloid beta pathology was associated with less anxiety and more risky behaviors. However, after prolonged antibody treatment, the mice avoided the open arms because their fear of heights and open spaces had been restored.
After examining the mice’s brains, the researchers noted that the behavioral changes coincided with a decrease in amyloid beta pathology. There were fewer plaques that caused severe neuronal swelling and more inert plaques. This shift in the neurotoxicity of plaques resulted in a reduction of swollen and degenerating axons and dendrites. However, the overall amount of plaque was not changed.
Surprisingly, the antibody treatment did not result in more microglia surrounding amyloid plaques. Instead, there was a change in how the microglia behaved. Microglia monitor their environment by extending arm-like processes into their surroundings. Antibody treatment increased the length of their arms, suggesting that the microglial could better surveil their surroundings. There was also an increase in the amount of amyloid beta being ingested by the microglia.
“The surprise, which perhaps should not be much of a surprise,” explained Colonna in an ALZFORUM interview, “is we saw a decrease in microglial clustering around plaques. It seems that as we reduced the toxicity of plaques, a secondary response was a reduction of microglia. Essentially, we reduced microgliosis.”
In other words, by decreasing amyloid beta toxicity, the antibody also decreased microglial clustering and inflammation. The most encouraging aspect of this study is that the treatment was beneficial despite ongoing amyloid beta aggregation and the presence of amyloid beta plaques. This treatment may be helpful even if administered at later stages of the disease.
A variant of the TREM2 antibody (AL002) has been tested in a first-in-human Phase I clinical trial, which tests the safety and side effects of the treatment in a small number of people. The treatment was well tolerated and did not have any serious adverse effects. The antibody’s activity could be confirmed by measuring the levels of biomarkers in the cerebrospinal fluid. Based on the results of the preclinical mouse models and the successful Phase I clinical trial, TREM2 antibodies show promise as an AD therapy.
Marco Colonna, M.D., Washington University School of Medicine in St. Louis
Published in:
Journal of Experimental Medicine
ALZFORUM Paper
https://www.alzforum.org/news/research-news/mice-activating-trem2-tempers-plaque-toxicity-not-load





