Posted January 8, 2014
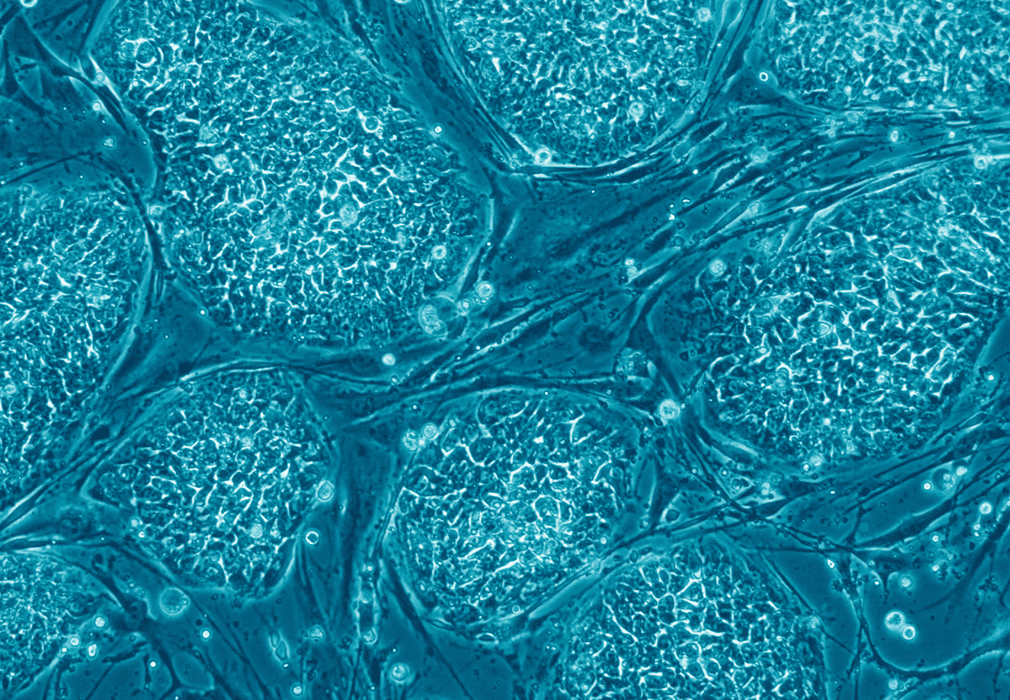
Scientists at The New York Stem Cell Foundation (NYSCF) Research Institute, working in collaboration with scientists from Columbia University Medical Center (CUMC), for the first time generated induced pluripotent stem (iPS) cells lines from non-cryoprotected brain tissue of patients with Alzheimer’s disease.
These new stem cell lines will allow researchers to “turn back the clock” and observe how Alzheimer’s develops in the brain, potentially revealing the onset of the disease at a cellular level long before any symptoms associated with Alzheimer’s are displayed. These reconstituted Alzheimer’s cells will also provide a platform for drug testing on cells from patients that were definitively diagnosed with the disease. Until now, the only available method to definitively diagnose Alzheimer’s disease that has been available to researchers is examining the brain of deceased patients. This discovery will permit scientists for the first time to compare “live” brain cells from Alzheimer’s patients to the brain cells of other non-Alzheimer’s patients.
NYSCF scientists successfully produced the iPS cells from frozen tissue samples stored for up to eleven years at the New York Brain Bank at Columbia University.
This advance, published today in Acta Neuropathologica, shows that disease-specific iPS cells can be generated from readily available biobanked tissue that has not been cryoprotected, even after it has been frozen for many years. This allows for the generation of iPS cells from brains with confirmed disease pathology as well as allowing access to rare patient variants that have been banked. The stem cell lines generated for this study included samples from patients with confirmed Alzheimer’s disease and four other neurodegenerative diseases.
This important advance opens up critical new avenues of research to study cells affected by disease from patients with definitive diagnoses. This success will leverage existing biobanks to support research in a powerful new way.
iPS cells are typically generated from a skin or blood sample of a patient by turning back the clock of adult cells into pluripotent stem cells, cells that can become any cell type in the body. While valuable, iPS cells are often generated from patients without a clear diagnosis of disease and many neurodegenerative diseases, such as Alzheimer’s disease, often lack specific and robust disease classification and severity grading. These diseases and their extent can only be definitively diagnosed by post-mortem brain examinations. For the first time we will now be able to compare cells from living people to cells of patients with definitive diagnoses generated from their banked brain tissue.
Brain bank networks, which combined contain tens of thousands of samples, provide a large and immediate source of tissue including rare disease samples and a conclusive spectrum of disease severity among samples. The challenge to this approach is that the majority of biobanked brain tissue was not meant for growing live cells, and thus was not frozen in the presence of cryoprotectants normally used to protect cells while frozen. NYSCF scientists, in collaboration with CUMC scientists, have shown that these thousands of samples can now be used to make living human cells for use in disease studies and to develop new drugs or preventative treatments for future patients.
NYSCF stem cell researcher Scott Noggle, Ph.D., the Charles Evans Senior Research Fellow for Alzheimer’s Disease and CUMC physician-scientist John Crary, M.D., Ph.D., are the senior authors and NYSCF researchers Andrew Sproul, Ph.D., and Lauren Vensand are the co-first authors of this study.
The New York Stem Cell Foundation research was supported by the Cure Alzheimer’s Fund, Charles Evans Foundation, and The New York Stem Cell Foundation. The Columbia University Medical Center research was funded by the Alzheimer’s Association (NIRG-11-204450), the Louis V. Gerstner, Jr., Foundation, and The American Recovery and Reinvestment Act (ARRA) funds through Grant number P30AG036453.