Posted January 8, 2014
A stem cell model of familial Alzheimer’s disease (FAD) was successfully generated in a recent study, allowing researchers to identify 14 genes potentially implicated in the disease. One gene in particular demonstrates the important role inflammation may play in the brain of Alzheimer’s patients. The study was completed by scientists at The New York Stem Cell Foundation (NYSCF) Research Institute in collaboration with scientists at the Icahn School of Medicine at Mount Sinai (ISMMS) and funded in part by the Cure Alzheimer’s Fund (CAF).
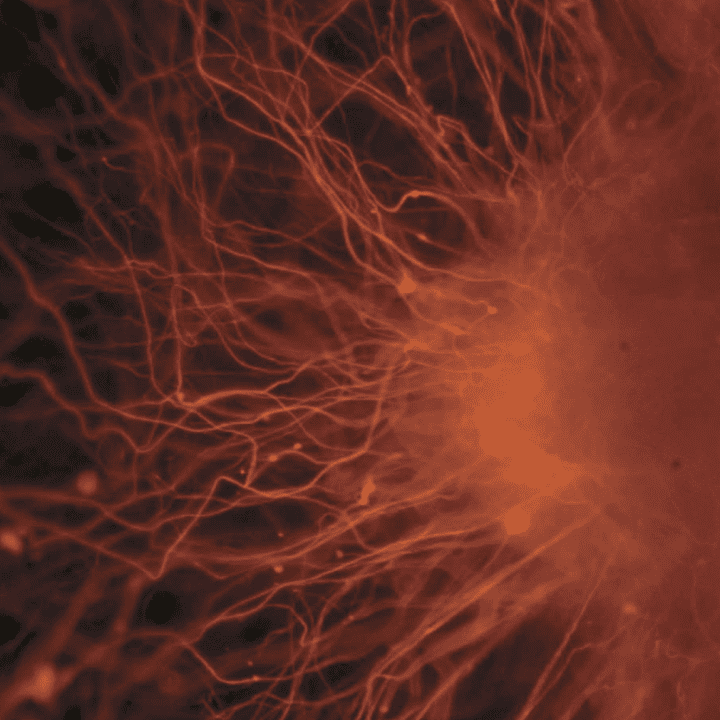
In the study published today in PLOS ONE, a team of scientists produced stem cells and neural precursor cells (NPCs), representing early neural progenitor cells that build the brain from patients with severe early-onset AD with mutations in the Presenilin 1 (PSEN1) gene. These NPCs had elevated Abeta42/Abeta40 ratios, indicating elevation of the form of amyloid found in the brains of Alzheimer’s patients. These levels were greater than those in adult cells that did not have the PSEN1 mutation. This elevated ratio shows that the NPCs grown in the petri dish accurately reflected the cells in the brains of FAD patients.
“The gene expression profile from the familial Alzheimer’s stem cells points to inflammation, which is especially exciting because we would not usually associate inflammation with this particular Alzheimer’s gene,” said Sam Gandy, M.D., Ph.D., Professor of Neurology and Psychiatry and Director of the Center for Cognitive Health at the Icahn School of Medicine at Mount Sinai and a co-author on the study. Gandy is also Associate Director of the NIH-Designated Mount Sinai Alzheimer’s Disease Research Center and leader of the Cure Alzheimer’s Fund Stem Cell Consortium.
“This is the kind of innovative science that will help us better understand the cause of Alzheimer’s and how to approach the disease with effective therapies,” said Tim Armour, President and CEO of Cure Alzheimer’s Fund. “It also showcases how targeted investment of critical resources can make a difference in finding solutions to this debilitating disease.”
The researchers generated induced pluripotent stem (iPS) cells from affected and unaffected individuals from two families carrying PSEN1 mutations. After thorough characterization of the NPCs through gene expression profiling and other methods, they identified 14 genes that behaved differently in PSEN1 NPCs relative to NPCs from individuals without the mutation. Five of these targets also showed differential expression in late onset Alzheimer’s disease patients’ brains. Therefore, in the PSEN1 iPS cell model, the researchers reconstituted an essential feature in the molecular development of familial Alzheimer’s disease.
The study’s co-lead authors Sam Gandy, M.D., Ph.D. and Scott Noggle, Ph.D. are both members of CAF’s Stem Cell Consortium, which supported this research. The Stem Cell Consortium is an international group of scientists collaborating on innovative research that investigates, for the first time, the brain cells from individuals with the common form of Alzheimer’s disease. Other members of the Consortium include Kevin Eggan, Ph.D., of Harvard University, Marc Tessier-Lavigne, Ph.D., of Rockefeller University, Doo Yeon Kim, Ph.D., of Harvard Medical School, and Tamir Ben-Hur, M.D., Ph.D., of Hadassah University.
Stem cells are the least mature cells in the body. This means they can be treated with a defined cocktail of factors that can cause maturation of cells along discrete cell types. With iPS cells, which are cells that can become any cell type in the body, it now is possible to take skin cells from adults and return them to an immature state. By redirecting skin cells from Alzheimer’s patients and turning them into nerve cells, investigators are able to study adult Alzheimer’s neurons (nerve cells) in the lab.
Although the majority of Alzheimer’s disease cases are late onset and likely result from a mixture of genetic predisposition and environmental factors, there are genetic forms of the disease that affect patients at much earlier ages. PSEN1 mutations cause the most common form of inherited familial Alzheimer’s disease and are one hundred percent penetrant, resulting in all individuals with this mutation getting the disease.
Identifying genes that behaved differently in patients with the mutation provides new targets to further study and better understand their effects on the development of Alzheimer’s disease. One of these genes, NLRP2, is traditionally thought of as an inflammatory gene.
“The fact that the NLRP2 gene is upregulated in these cells is interesting because inflammatory genes have long been implicated in late onset and sporadic forms of the disease. The importance is still unknown, but these cells may provide a platform to understand the function of this gene as well as others that contribute to Alzheimer’s disease,” said Scott Noggle, Ph.D., NYSCF – Charles Evans Senior Research Fellow for Alzheimer’s Disease and Director of the New York Stem Cell Foundation (NYSCF)’s laboratory and co-lead author on the study.
While other groups have recently generated human iPS cells models of Alzheimer’s disease with studies primarily focused on familial Alzheimer’s disease neurons, none of these studies addressed whether there are any differences between Alzheimer’s disease and control neural progenitor cells prior to neuronal differentiation.
Studying neural progenitor cells may also reveal developmental components of familial Alzheimer’s disease, and are more homogenous than the wide variety of neurons currently produced by differentiation protocols, which allows for better comparisons between controls and disease cells.
NYSCF stem cell researcher Andrew Sproul, Ph.D., a staff scientist at the NYSCF Research Institute was the first author on this study. Along with NYSCF and ISMMS researchers, scientists at Columbia University and the James J. Peters VA Medical Center made significant contributions to this study.
The New York Stem Cell Foundation Research was supported by grants from the Charles Evans Foundation, Alzheimer’s Drug Discovery Foundation, and NY Community Trust. Scott Noggle and Sam Gandy are jointly supported by NIH grant RF1AG042965 and the Cure Alzheimer’s Fund and the other ISMMS research was supported by the American Health Assistance Foundation.