Featured Researcher: William Mobley, M.D., Ph.D.
Distinguished Professor and Chair of the Department of Neurosciences at University of California, San Diego; Executive Director of UCSD’s Down Syndrome Center for Research and Treatment; Florence Riford Chair for Alzheimer’s Disease Research.
Born in landlocked Nebraska, William Mobley discovered the wonders of research when he first studied a sea cucumber’s hemoglobin. Now a prominent academic neurologist and the newest member of Cure Alzheimer’s Fund’s Scientific Advisory Board, Mobley’s passion for science and for living life never has waned.
Early days
William Mobley was born and raised in Lincoln, Nebraska. He was the fourth of five children and, despite having two hardworking parents, grew up without much money. “My mom had a part-time sales job and my dad sold coffee,” says Mobley. “He had been accepted to medical school, but couldn’t go because just as he was entering, his family lost everything in the crash of 1929. He became a milkman, and later a salesman.”
Education
Mobley attended the University of Nebraska-Lincoln, where he majored in chemistry and zoology and attained membership in Phi Beta Kappa. It was there where he first became interested in research. He wanted to go to a first-rate medical school, but the possibility appeared remote given his family’s financial position. When he learned students chosen for M.D. and Ph.D. programs had their educations paid for, he volunteered to work in a lab. Over spring break he went to Florida to observe sea cucumbers in tide pools and bring samples home to extract the hemoglobin present in their central cavity. “That’s when my love affair with research first began.” At the time, Mobley was torn between becoming a researcher or a doctor. Ultimately, he would become both.
The summer after his senior year he worked on hemoglobin at Einstein Medical School in New York. “I couldn’t wait to get to work in the morning,” he remembers. That long summer confirmed his commitment to research. In 1970, Mobley moved to the West Coast and began studying at Stanford University Medical School, where he worked in the lab of researcher Eric Shooter, whose earlier work had been on hemoglobin. “Eric was a great mentor,” says Mobley, “but he had shifted his focus to another protein”—nerve growth factor (NGF), a small protein with dramatic effects on neurons. When it became clear that working on NGF was going to be more exciting, Mobley switched to this protein.
Mobley married his wife Gretchen in 1972, earned his Ph.D. in neuro- and behavioral science in 1974 and his M.D. in 1976, and was a resident in pathology, pediatrics and neurology for the next six years. He and his family (including two little boys) moved to Baltimore for his neurology residency at Johns Hopkins University. “At the time, the Hopkins salary wasn’t enough to live on,” says Mobley. “So I joined the Army as a captain for three years (1982–1985), as part of a civilian residency program, and afterward served at the Walter Reed Army Institute of Research, just down the road in D.C.”
Alzheimer’s Disease and Down Syndrome
At Hopkins, colleagues discovered that cholinergic neurons, a certain set of neurons at the base of the brain, showed shrinkage and death in the brains of people with Alzheimer’s disease (AD). “It was the first such group of neurons shown to be vulnerable in AD,” says Mobley. Shortly thereafter NGF joined the Alzheimer’s scene. “We followed the lead of Franz Hefti and his colleagues and were the first to state unequivocally that NGF acted on these neurons and that it likely served as a neurotrophic factor in the brain. And it turned out we were right,” he says.
“Studying the brain was much more fun than hemoglobin,” says Mobley. “But the underlying theme that captured me was similar. I’m fascinated by the biochemical interaction of proteins in the context of their local environment—how hemoglobin changes shape when it binds oxygen, how neurotrophic factors signal within neurons and how the brain changes as it learns.” But studying brain disorders in the late 1980s was not easy, as few animal models existed at that time. “Ideally we wanted to study AD, but the only model suitable at that time was a model of Down syndrome (DS). So we decided to focus on the biology of AD in DS.”
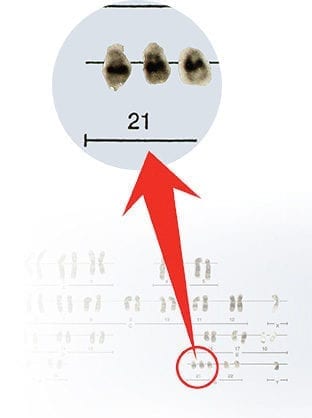
They soon discovered a disruption in NGF signaling in the DS models. People with DS are born with an extra copy of chromosome 21, which harbors the APP gene (a key protein in AD). Virtually all adults with DS develop AD pathology by age 40, and half develop dementia by age 50. Importantly, the extra copy of APP plays an important role in disrupting NGF trafficking within neurons and its signaling properties. “The goal is to find a way to restore the normal pattern of growth factor trafficking and signaling in hopes of preventing Alzheimer’s disease in people with DS.”
After completing his residency in 1985, Mobley moved back to the West Coast, working at the University of California, San Francisco; Stanford University; and UCSD, where he’s been since 2009.
Current work
Today, Mobley’s research on the neurobiology of DS has brought new insights into the condition, including possible treatments. He has done pioneering work on the neurobiology of AD using a DS mouse model that has paved the way for ongoing studies of AD in experimental models. “If you really focus on a singular topic—in this case, cognition and Down syndrome—it allows you the freedom to think about things from different angles,” says Mobley. “APP is clearly very important. Now we can really study it, understand how it works and figure out how to stop it from working. My special hope is that by studying Down syndrome, we’ll be able to help everyone with Down syndrome and Alzheimer’s. That’s a big part of what Cure Alzheimer’s Fund can help us with, and I’m very proud of what they’re doing.”