Over the past few years, our understanding of Alzheimer’s disease has increased immensely. We can now identify three distinct parts of the disease pathology: early-stage Abeta (amyloid) accumulation, mid-stage development of tau tangles, and late-stage inflammation.
Scientists on our Research Consortium are investigating all three of these points of intervention. On March 6, we talked to Drs. Steven Wagner, David Holtzman, and Rudy Tanzi about how their labs are working to stop Alzheimer’s in its early, middle, and late stages.
Early-Stage Intervention: Abeta
Steven Wagner, Ph.D.
University of California, San Diego
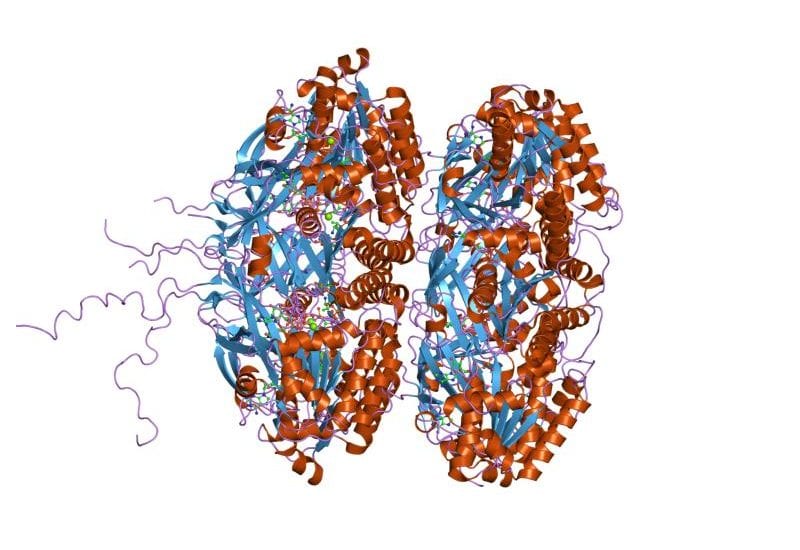
The Abeta protein has long been recognized as central to the development of Alzheimer’s pathology. Only recently, however, have we come realize that this substance not only causes problems in Alzheimer’s patients, but also plays an important role in the innate immune system. Dr. Steven Wagner is working to produce a drug that will modulate an enzyme called gamma secretase, which is a critical contributor to Abeta production. By regulating rather than eliminating Abeta, Wagner and his lab hope to safely halt the development of Alzheimer’s in its early stages.
Middle-Stage Intervention: Tau
David Holtzman, M.D.
Washington University in St. Louis
In addition to Abeta, tau tangles, another abnormal aggregation of proteins, are known to cause damage in the Alzheimer’s brain. Dr. Holtzman has recently demonstrated breathtakingly positive results in a proof-of-concept study using antibodies, aimed at stopping the aggregation and spread of tau.
Late-Stage Intervention: Inflammation
Rudy Tanzi, Ph.D.
Harvard Medical School/Massachusetts General Hospital
The plaques and tangles of the early and middle stages of Alzheimer’s trigger an immune response, which under normal circumstances would help to clear away damaged and unwanted cells. When the cells responsible (microglia) do not function properly, damaging inflammation occurs – “friendly fire” that greatly exacerbates the disease pathology in a vicious cycle. Dr. Tanzi is researching a gene called CD33 that, when deactivated, helps microglial cells to stop this cycle.